Various studies from the last 60 years have established the health benefits of specific compounds and the adverse effects of diets poor in certain micronutrients. Here are just a few of them:
- A 2002 review of almost 40 years of research summarized knowledge about the role of different vitamins in preventing such chronic conditions as cardiovascular disease, various types of cancer, and osteoporosis [1]. Studies cited showed how inadequate intake of folate and vitamins B6 and B12 was associated with increased risks for coronary heart disease [2], cognitive decline, and carcinogenesis.
- The antioxidant effects of vitamin E are known to prevent oxidative damage to lipid membranes, the main factor affecting the aging of the skin. On the other hand, clinical manifestations of vitamin E deficiency include muscle weakness and ataxia, a group of disorders that affect coordination, balance, and speech.
- Vitamin D deficiency, which is more common than you might think, is associated with bone loss, osteoporosis, and increased risk of fractures [3].
- Deficiencies of vitamin A, which is necessary for proper vision and organ formation, can lead to xerophthalmia, night blindness, and increased susceptibility to disease.
- Patients with a low intake of vitamin K, a requirement for proper bone development, can experience poor clotting or even hemorrhaging [4].
- Magnesium deficiency is associated with colorectal and other cancers, hypertension, osteoporosis, and diabetes [5].
Vitamins are organic compounds produced by plants and animals, while minerals are inorganic and exist in soil and water. When we eat, we consume the vitamins plants or animals have synthesized and the minerals they have absorbed. For millennia, this was the only way humans could access these essential micronutrients.
The change in modern thinking about how to acquire micronutrients came when Dr. Linus Pauling, the two-time Nobel laureate, published his 1970 book Vitamin C and the Common Cold. Pauling’s writings introduced the therapeutic properties of vitamins to a wide audience and popularized the use of vitamin tablets and nutritional supplements. A 2019 consumer survey found that 77 percent of U.S. individuals take dietary supplements, with most popular being vitamin D, calcium, and fish oil [6].
Multivitamin complexes “tailored” to different age groups and population cohorts may seem like a great fix for any deficiencies in any person’s diet, but some researchers have demonstrated that the dietary intake of micronutrients may trump supplements in terms of its efficiency.
In one 2007 study of both the dietary and the supplemental intake of calcium in postmenopausal women, the group that received calcium from their diet or from diet and supplements had “significantly greater” bone mineral density (BMD) than those who obtained calcium primarily from the supplements [7]. This difference was especially pronounced in those who acquired the mineral primarily from their diet, even though their total calcium intake was lower than that of those who took the supplements.
A 2014 review of several clinical trials compared the effects of whole food (in the form of tomato-based products) and supplemental intake of lycopene on intermediate cardiovascular disease (CVD) risk factors, including oxidative stress, inflammation, and high blood pressure. While the study recommended lycopene in a supplemental form for blood pressure management, tomato intake provided more favorable results on cardiovascular risk endpoints than the supplements [8].
An overall preference for dietary intake of micronutrients over supplements was also the conclusion of a 2005 review of numerous cohort studies and clinical trials entitled “Micronutrients: dietary intake v. supplement use.” The article found that “classic micronutrient-supplementation randomized controlled intervention trials have largely failed to show an effect on chronic disease risk.”
At the same time, various cohort studies, including those investigating the effects of a Mediterranean diet rich in fruit and vegetables and focused on reduced fat intake found a reduction in overall mortality risks and the prevalence of coronary heart disease. Researchers hypothesize that vitamin and mineral supplements may not be enough if they are used by someone with an energy-rich and micronutrient-deficient diet. Fruits and vegetables contain more than just one micronutrient and provide a more complex mixture of these compounds, which may, in turn, have greater beneficial effects than simply ingesting large doses of specific vitamins [9].
An overreliance on certain vitamins and minerals can also have adverse health effects [10]. In particular, excess vitamin A intake may lead to liver damage and increased risks of hip fracture. Excessive use of selenium can lead to gastrointestinal disorders, hair loss, fatigue, and neurological damage, while too much iodine may cause thyroid hyperactivity.
The beauty of our AI-powered Abe-Health algorithms is that they can help you correct for both the deficits AND the excesses of micronutrients.
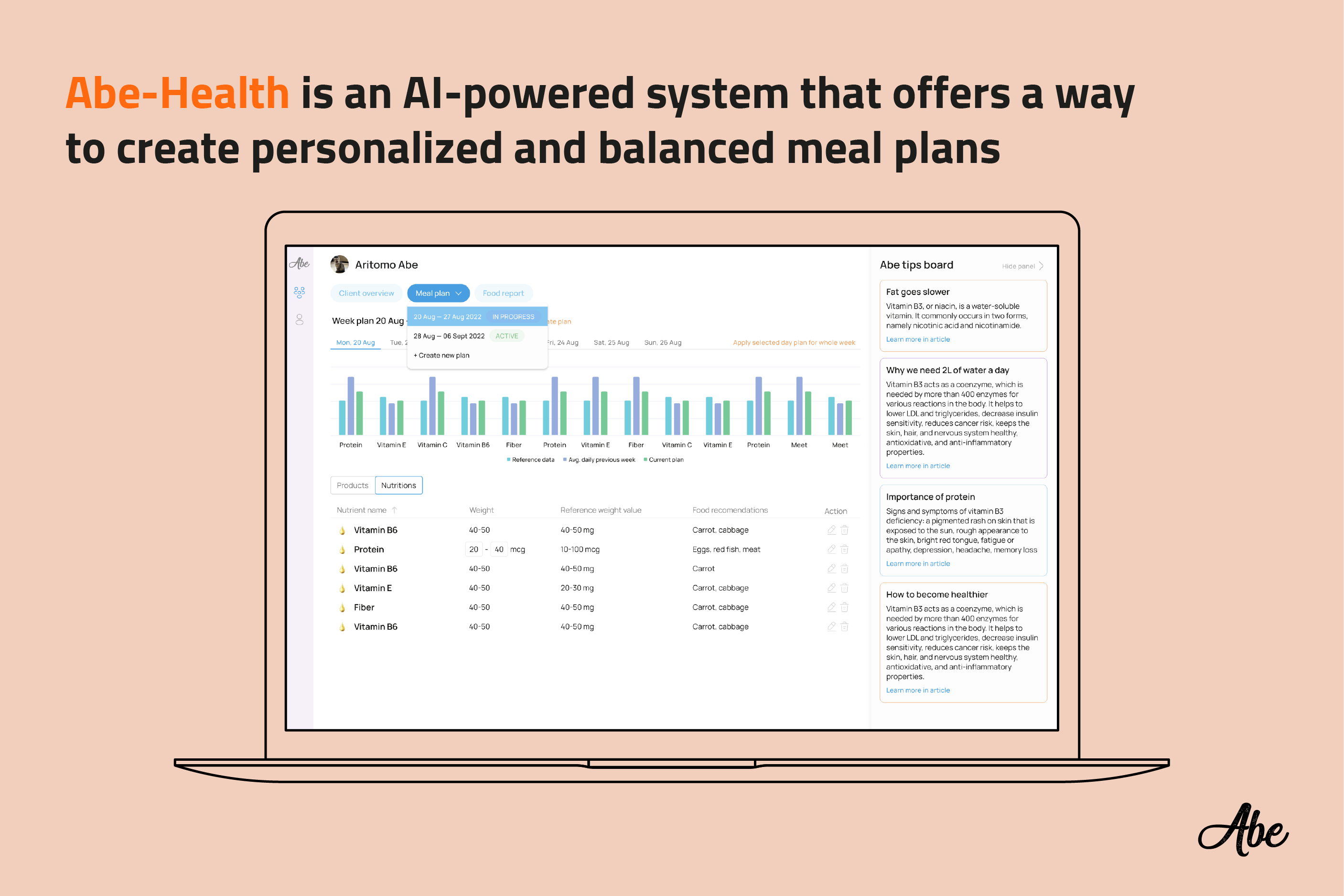
Whether you’re a nutritionist, a health coach, a personal trainer, or any other type of health consultant, Abe offers a way to create personalized and balanced meal plans for your clients. Professionals can easily track their clients’ progress and suggest alternatives when somebody veers off track.
When you create a meal plan using Abe-Health, it identifies the most in-deficit vitamins and minerals and alerts you to the risks those deficits present. The AI-powered system suggests products that can compensate for these shortages and balance the person’s diet. These interventions will ensure the micronutrients are added to the diet in the form of actual food, not supplements, and guarantee the most beneficial effects possible for the person’s short-term and long-term health.
With a variety of products to choose from for all the major nutrients, you can create meal plans tailored specifically to each client, both in terms of micronutrient profile and taste preference. This personalization will both please your clients and make their success more likely.
1. Robert H. Fletcher, MD, MSc; Kathleen M. Fairfield, MD, DrPH. Vitamins for Chronic Disease Prevention in Adults. JAMA. 2002;287(23):3127-3129. Link.
2. Graham IM, Daly LE, Refsum HM, et al. Plasma homocysteine as a risk factor for vascular disease: the European Concerted Action Project. JAMA. 1997; 277:1775-1781. Link.
3. Lips P. Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocrinology Review. 2001; 22:477-501. Link.
4. Ansell JE, Kumar R, Deykin D. The spectrum of vitamin K deficiency. JAMA. 1977; 238:40-42. Link.
5. Ames Bruce N. Low micronutrient intake may accelerate the degenerative diseases of aging through allocation of scarce micronutrients by triage. PNAS. 2006; 103 (47): 17589-17594. Link.
6. Dietary Supplement Use Reaches All Time High. Council for Responsible Nutrition (CRN) Survey. 2019. Link.
7. Napoli N, Thompson J, Civitelli R, Armamento-Villareal R. Effects of dietary calcium compared with calcium supplements on estrogen metabolism and bone mineral density. The American Journal of Clinical Nutrition. 2007; 85 (5): 1428-1433. Link.
8. Burton-Freeman B, Sesso H. Whole Food versus Supplement: Comparing the Clinical Evidence of Tomato Intake and Lycopene Supplementation on Cardiovascular Risk Factors. Advances in Nutrition; 5 (5): 457-485. Link.
9. Woodside J, McCall D, McGartland C, Young I. Micronutrients: dietary intake v. supplement use. The Proceedings of the Nutrition Society. 2005; 64(4): 543-553. Link.
10. Verkaik-Kloosterman J, McCann M, Hoekstra J, Verhagen H. Vitamins and minerals: issues associated with too low and too high population intakes. Food and nutrition research. 2012; 56: 10.3402. Link.
